Distinct Neurobiological Signatures of Early-Stage Depression and Psychosis
Post by Shalana Atwell
The takeaway
Neurobiological signatures can distinguish early-stage depression and psychosis and may help uncover mechanistic pathways and guide targeted interventions.
What's the science?
Immune system alterations have been repeatedly linked to mood and psychotic disorders. Previous research has identified distinct and overlapping inflammatory markers in depression and psychosis whose dysregulation is associated with changes in brain gray matter volume (GMV). However, we need a more holistic view of the anatomical changes and inflammatory markers that are related to distinct pathologies of depression and psychosis. Furthermore, the complex relationship between immune factors and GMV makes univariate approaches poorly suited to capture higher-order patterns. Recently, in JAMA Psychiatry, Popovic and colleagues aimed to determine if multivariate patterns linking peripheral inflammatory markers with whole-brain gray matter volume could (1) distinguish early-stage depression and psychosis and (2) reveal how clinical factors such as childhood trauma and cognition relate to these biological signatures.
How did they do it?
The authors analyzed baseline data from individuals with recent-onset depression, recent-onset psychosis, clinical high-risk state of psychosis, and healthy controls. All groups were medication-naïve or minimally medicated to reduce the confounding effects of antipsychotics and antidepressants. Peripheral blood was assayed for a panel of inflammatory and related markers such as interleukin (IL), tumor necrosis factor-alpha (TNF- α), and C-reactive protein (CRP), to name a few. These protein readouts were combined with demographic and technical covariates (age, sex, BMI, study group, MRI image quality) into a ‘blood’ domain. The ‘brain’ domain was generated using voxelwise gray matter volume (GMV) maps from structural MRI, which were mapped onto anatomical and functional network atlases to interpret where in the brain the signatures were expressed. To identify multivariate brain-blood domain relationships, the authors utilized sparse partial least squares regression (SPLS), which generates latent variables (LVs) that maximize covariance between the blood markers and GMV voxels. Each LV consists of weight vectors for blood markers and GMV voxels. Individual scores were computed by projecting each person’s data onto these weight vectors, and the correlation between blood and brain scores quantified how strongly the LV captures shared variance. Next, the authors used machine learning (linear support vector machine classification – SVM-C) to test whether life history (e.g., childhood trauma), cognitive function, and medications could predict high vs low expression of the psychosis-related and depression-related signatures.
What did they find?
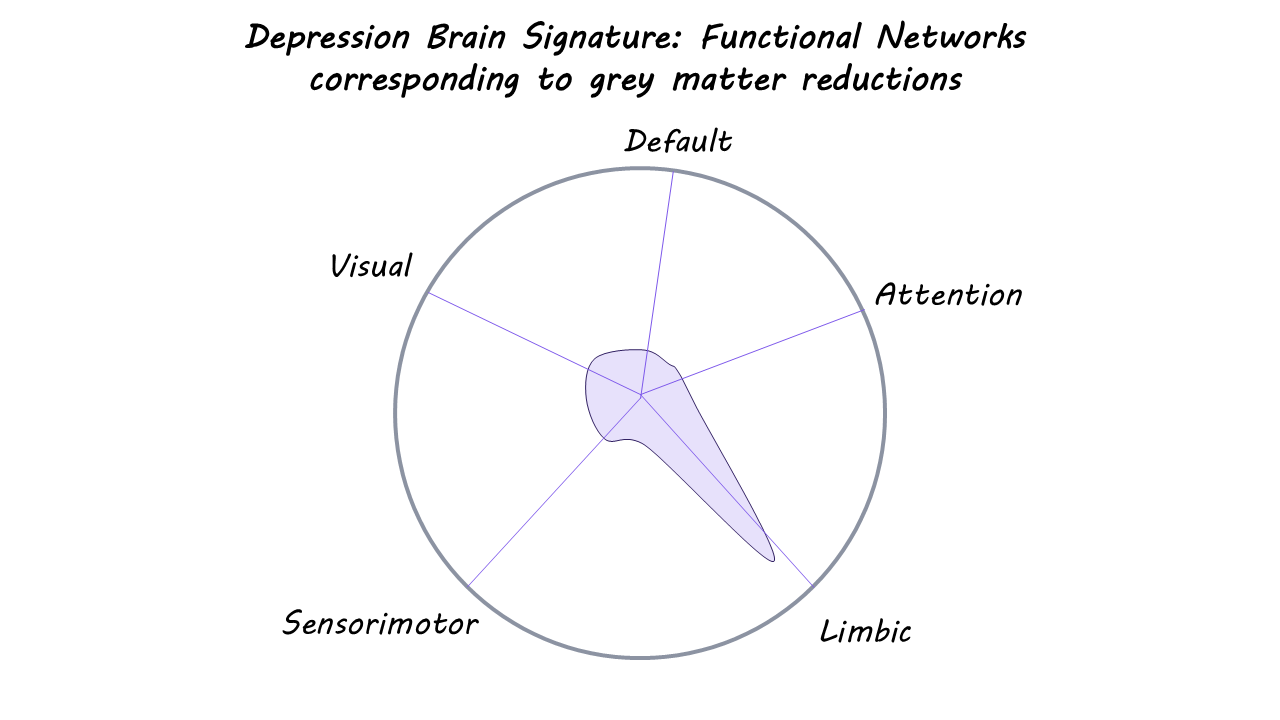
The authors found two significant brain-blood signatures that indicated a separation of psychotic and depressive disorders. Those with clinical high-risk status had higher levels of CRP compared to recent-onset psychosis, while recent-onset psychosis was associated with higher age, BMI, and certain inflammatory proteins (IL-6 and TNF- α). Additionally, they found disruptions in GMV mainly in cortico-thalamo-cerebellar circuitry that supports sensory integration and salience attribution. These findings suggest a different immune profile in high-risk and psychosis groups, as well as circuit disruptions that might serve as a neurobiological marker for defining different states of psychosis. In the depression signature, recent-onset depression was associated with higher levels of a mix of pro- and anti-inflammatory proteins (IL-1RA, IL-4, S100B, IL-1β, IL-2, and BDNF) and reductions in GMV in limbic system structures, such as the hippocampus and amygdala, compared to healthy controls. These findings support a complex immune-inflammatory and compensatory response as well as limbic-cortical dysregulation as a core neurobiological feature of depression.
What's the impact?
This study is one of the first large, minimally medicated, transdiagnostic investigations to show that early-stage depression and psychosis are associated with distinct multivariate immune-brain signatures. Furthermore, the authors demonstrate that these signatures are shaped by childhood trauma and cognition, supporting stage-specific differentiation of psychosis and depression, which could guide targeted early interventions.