Neural Signature of Recovery Following Traumatic Brain Injury
Post by Shalana Atwell
The takeaway
The extent of functional recovery from moderate to severe traumatic brain injury (TBI) in individual patients can be challenging to predict accurately. This research found that individuals with normal ‘on-off’ toggling (anticorrelation) between key brain networks following TBI are more likely to have a favorable functional recovery.
What's the science?
Current clinical models used to predict functional outcomes after TBI rely on age, extent of injury, motor scores, and the presence of other illnesses. Still, these predictive models do not account for neuroanatomical location or functional integrity of brain networks. Prior studies have used resting state functional magnetic resonance imaging (rs-fMRI) to measure functional connectivity (how brain regions communicate) in TBI studies. However, connectivity measures were inconsistent, and no model derived from fMRI data has been able to predict functional outcomes following TBI across independent datasets. Recently, in PNAS, Snider and colleagues investigated whether rs-fMRI can predict functional outcomes 6 months following injury across independent studies, as well as interrogated whether the predictive capacity of these measures is on par with or exceeds current prognostic tools for TBI.
How did they do it?
The authors pooled data from three TBI studies where each participant had completed multiple brain scans [MRI, diffusion tensor imaging, and rs-fMRI] and a 6-month follow-up after injury that assessed functional dependence [Glasgow Outcome Scale–Extended]. Brain scans measured structure (MRI), as well as the strength of connections between different brain regions by analyzing correlations in their activity over time (rs-fMRI) and organization and structural integrity of white matter tracts (diffusion tensor imaging). They cleaned and standardized MRI [CONN toolbox] and diffusion tensor imaging data to correct for excessive motion, technical differences across studies, and poor scan quality.
Using one dataset, a model [logistic regression] tested the ability of 435 pairs of connected brain regions to discriminate favorable vs unfavorable functional TBI outcomes. These pairs were validated using two-fold cross-validation and repeated testing to ensure results were not due to chance. The best-performing connections were combined into a predictive model and then tested on a separate dataset, confirming generalizability. They utilized brain connectivity patterns to predict recovery outcomes following TBI. Finally, the authors investigated whether adding MRI-based measures matched or improved predictions beyond the standard clinical scoring systems.
What did they find?
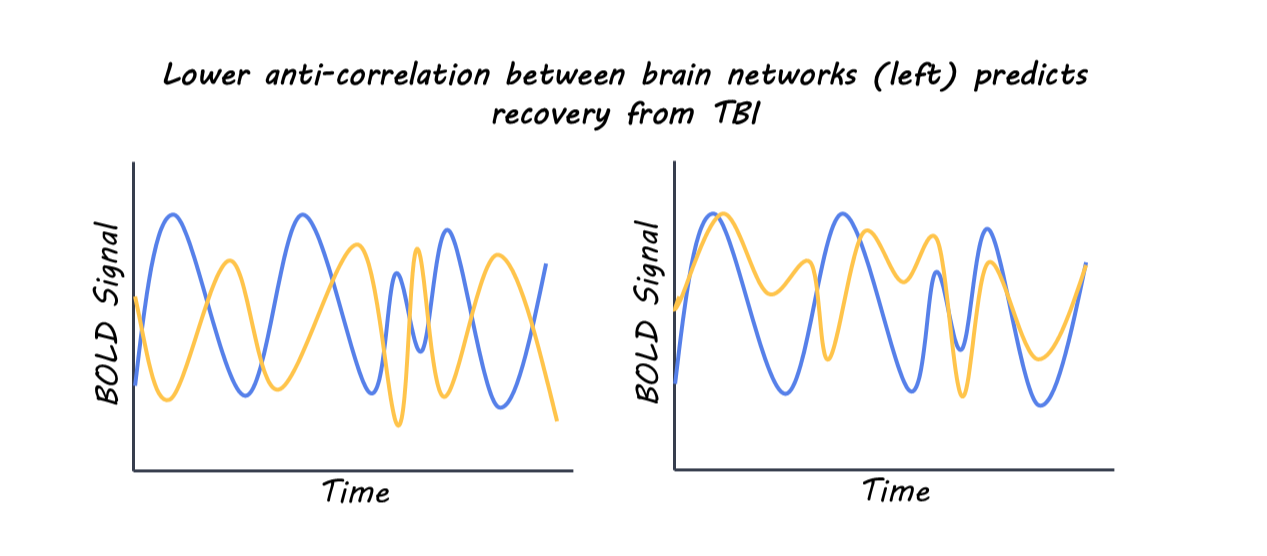
Using their model, they found that the strongest predictor of 6-month recovery was the functional anticorrelation (one network turns off when the other turns on) between the salience network’s left anterior insula and the default mode network’s right parietal region. Patients with more normal anticorrelation between networks following TBI were more likely to have better recovery at 6 months following injury. Adding two more connections—the frontoparietal network’s right lateral prefrontal cortex to the visual network and the language network’s right frontal gyrus to the default mode network’s medial prefrontal cortex—created a three-connection model that improved performance and predicted recovery with high accuracy across independent data sets. Incorporating two additional connections created a more accurate prognostic model. Finally, they combined the three-connections identified from rs-fMRI with standard clinical scoring systems, which yielded a significantly improved outcome prediction, showing higher sensitivity and specificity for identifying patients likely to recover. This highlights the possibility of augmenting predictive TBI scoring models with rs-fMRI data to refine treatment planning.
What's the impact?
This study identifies preservation of specific resting-state anti-correlations between brain networks as a strong marker of functional recovery following moderate to severe TBI. Changes in brain connectivity patterns after injury could be incorporated into clinical prognostic tools and possibly leveraged as a therapeutic target.