Deep Brain Stimulation as an Individualized Treatment for Depression
Post by Leanna Kalinowski
The takeaway
Depression is a psychiatric disorder that affects individuals differently, leading to difficulty in developing universal treatments. Researchers have successfully tested a new therapeutic strategy that uses individualized brain activity to guide treatment for depression with deep brain stimulation.
What's the science?
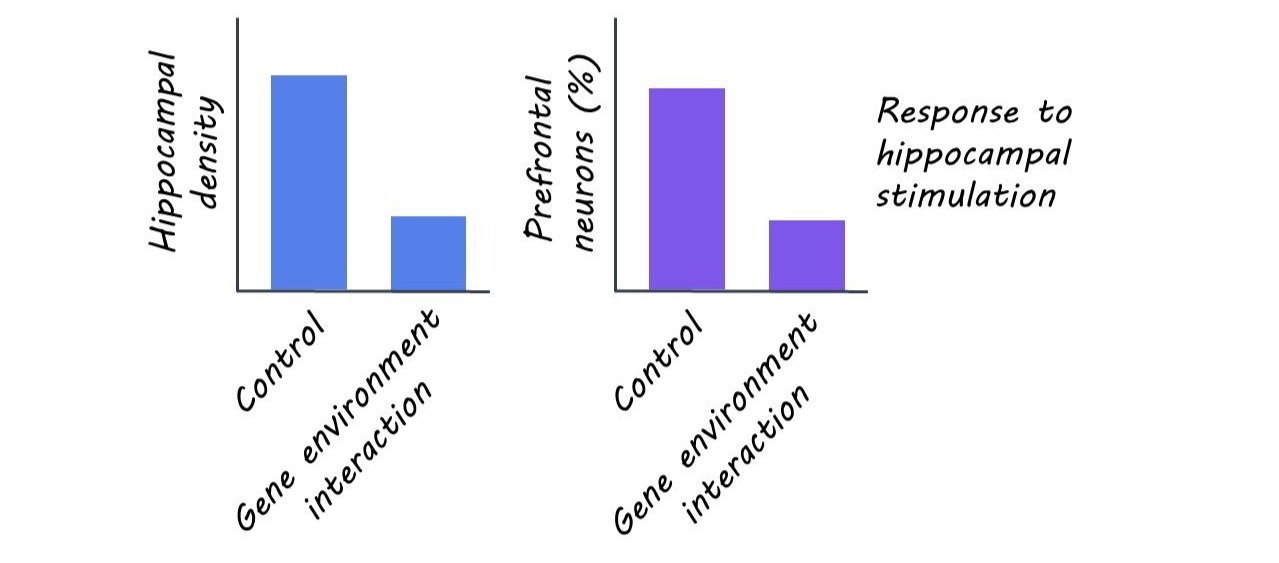
Deep brain stimulation (DBS) is a surgical procedure in which electrodes are implanted into the brain to deliver therapeutic electrical stimulation. It has shown success in treating movement disorders (e.g., Parkinson’s disease), which has led to a great interest in applying DBS to psychiatric disorders like treatment-resistant depression (i.e. depression that does not respond to medication). While preliminary studies on the effectiveness of DBS for treating depression showed promise, clinical trials were not as successful. This is likely due to depression being a highly heterogeneous disorder, highlighting a need for an individualized understanding of the specific brain regions contributing to a patient’s depressive symptoms. This week in Biological Psychiatry, Sheth and colleagues used intracranial recordings coupled with DBS to develop an individualized treatment strategy for depression.
How did they do it?
The researchers first surgically implanted two sets of electrodes into the brain: (1) DBS electrodes, to therapeutically stimulate the brain, and (2) stereo electroencephalography (sEEG) electrodes, to measure brain activity. The brain surgery was guided by an innovative holographic augmented reality platform to visualize the brain targets and their connections in 3D.
Following the first surgery, the researchers used the sEEG electrodes to take continuous recordings of the patient’s brain activity in an inpatient setting. During these recordings, the patient engaged in a variety of behavioral tasks designed to measure their mood state. The brain recordings, coupled with information about the patient’s mood state, then allowed for the researchers to calculate the personalized brain stimulation parameters most likely to produce an effective treatment outcome. Following these calculations, the patient underwent a second surgery to remove the sEEG electrodes and internalize the DBS electrodes. The patient then entered the outpatient phase of the trial, where they underwent eight months of DBS, after which they underwent a weekly gradual decrease in stimulation levels.
What did they find?
During the ten-day inpatient phase, the patient’s depression symptom scores rapidly improved. They reported a desired mood state on the ninth day of DBS which, in combination with computational methods, informed the stimulation parameters to be used for the remainder of the study. During the eight-month outpatient phase, the patient reported improvements in mood, increased interest in pleasurable activities, and closer emotional connections to loved ones. These subjective reports were accompanied by an improvement on depression symptom rating scales. Taken together, these results demonstrate the promising initial effectiveness of this approach in treating depressive symptoms. During the gradual discontinuation phase, the patient reported worsening mood, which was quickly reversed when DBS was reinstated. This suggests that symptom reduction was a true DBS-induced response and not a placebo effect.
What's the impact?
This study was the first to combine sEEG recordings with DBS, leading to a clinically effective personalized therapy for depression. This approach, if consistently demonstrated to be safe and effective, may be used to develop and improve future therapeutic strategies for other neurological and psychiatric disorders.