Brain Activity Associated with Positive Patient-Clinician Interaction
Post by D. Chloe Chung
What's the science?
Interaction between a patient and clinician can substantially impact therapeutic outcomes. For example, an unsatisfactory interaction can prevent patients from seeking medical care, but a positive patient-clinician interaction can actually lead to psychological relief of patients’ symptoms such as pain, amplifying benefits from the actual medical treatment. While it remains unclear what mechanisms underlie such phenomenon, several studies have emphasized the importance of synchronized behaviors and neural activity in social interactions such as bonding. This week in Science Advances, Ellingsen and colleagues used functional magnetic resonance imaging (fMRI) to demonstrate that social interaction between patients and clinicians can improve clinical outcomes by mirroring their behaviors and harmonizing neural activity in brain regions that regulate empathy.
How did they do it?
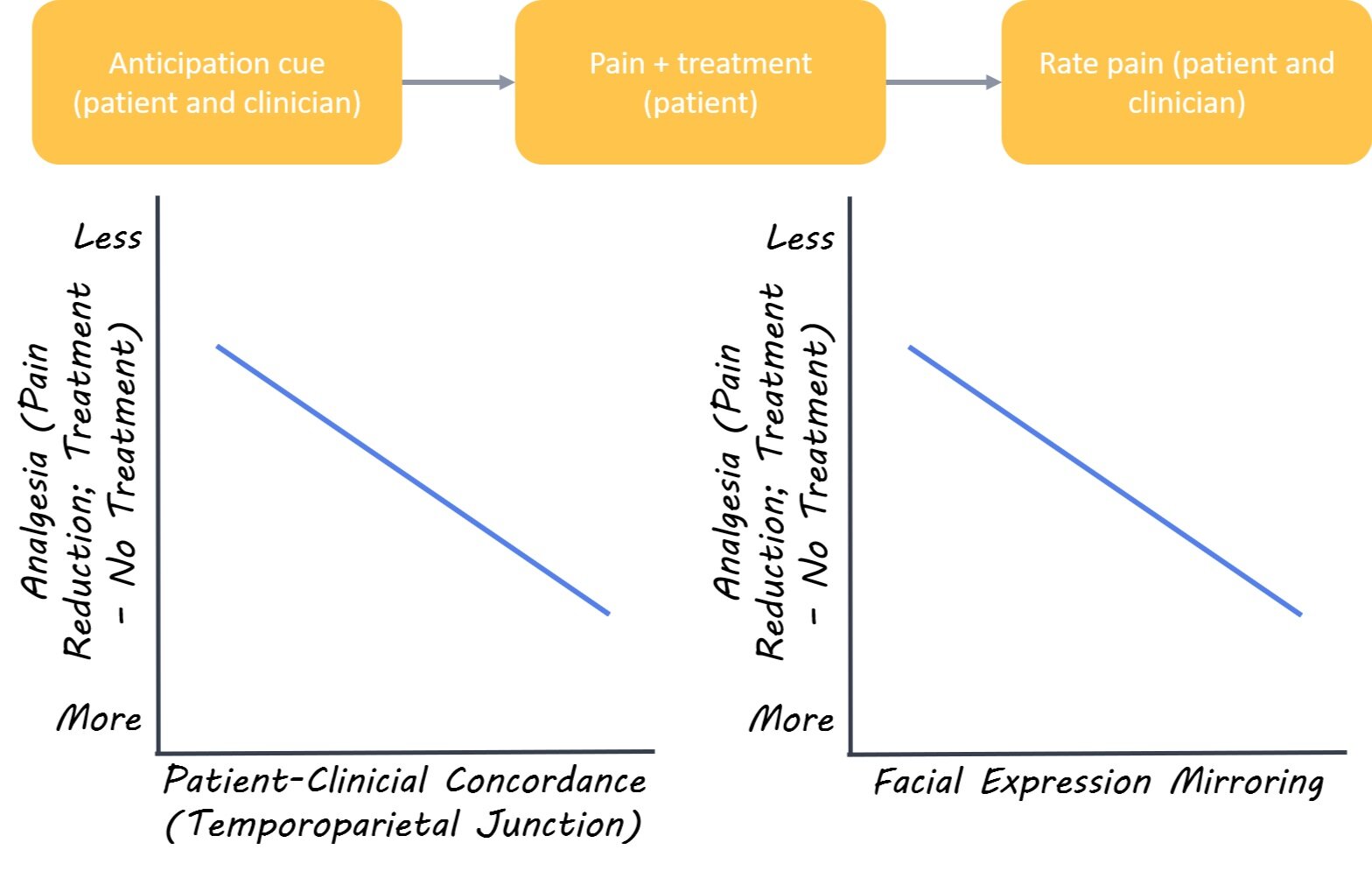
The authors recruited 23 fibromyalgia patients with chronic pain (all females) and 22 acupuncture clinicians (15 females) and matched them into 40 unique pairs. In the “clinical interaction” condition, the pair first established a rapport before the experiment (pain treatment) as the clinician gave consultation to the patient. In contrast, the pair in the “no interaction” control condition skipped the consultation and was only briefly introduced to each other before the experiment. On the day of the pain treatment, the patient and the clinician were placed in separate MRI scanners but were able to communicate with one another using facial expressions via video camera. Both participants received a visual cue to anticipate whether the patient would receive either a) treatment or b) no treatment following a moderate pressure pain evoked in the patient’s leg. Next, the clinician could press a button to give either real acupuncture treatment or a sham treatment to the patient’s leg. Both the clinician and patient were blind to whether a real treatment was given. After the trial, the pair were asked to rate the intensity of pain. The pair underwent 12 trials while their brain activity was scanned using fMRI
What did they find?
Both patients and clinicians reported less pain when the treatment was given, regardless of it being real or sham. Interestingly, video analysis of facial expressions revealed that patients tended to experience greater pain relief and stronger rapport with the clinician when the patients and the clinicians mirrored each other’s facial expressions. This suggests that social mirroring is linked to enhanced clinical outcomes. When the authors compared brain activity between groups they found that pairs from the “clinical interaction” group showed increased dynamic coupling of brain activity in the circuitry involved in social mirroring. In other words, the brain regions implicated in empathy were activated at the same time (i.e. concordant) in clinicians and patients if they already established a rapport prior to the pain treatment. Specifically, a brain area called the temporoparietal junction was activated at the same time in both pair members when they received an anticipation cue for treatment options. Upon further analysis, the authors found that concordance (co-activation between patient and clinician) of this brain region also led to greater pain relief via increased activity in a second brain region in the empathy neural circuitry that can also modulate pain.
What’s the impact?
This work sheds light on the neural circuitry involved in positive interactions between clinicians and patients. Further, this research demonstrates that positive patient-clinician interactions can improve clinical outcomes. The role of empathy in social interaction has been previously discussed in many studies, but this is the first to simultaneously monitor neural activity of two people who are interacting with each other in a clinical setting. Findings from this study may help guide clinicians in their interactions with patients to enhance clinical outcomes for patients.
Ellingsen et al. Dynamic brain-to-brain concordance and behavioral mirroring as a mechanism of the patient-clinician interaction. Science Advances (2020). Access the original scientific publication here.