Cognitive Network Processing in Chronic Pain
Post by Natalia Ladyka-Wojcik
The takeaway
The claustrum, a subcortical nucleus of the brain, may play an important role in both acute and chronic pain, such as the pain experienced by patients with migraines. This region is activated by painful stimulation and shows abnormal patterns of functional activity among migraine patients.
What's the science?
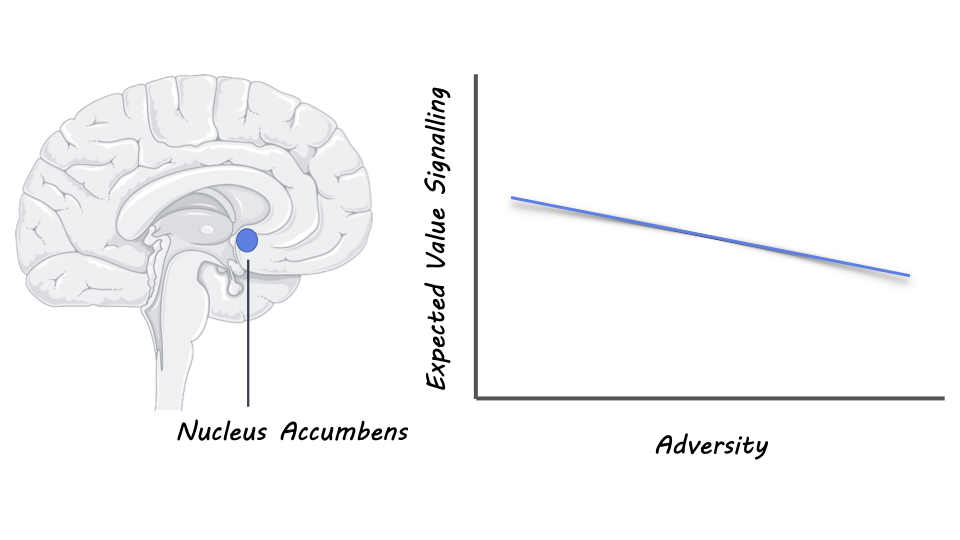
Patients who suffer from chronic pain often report difficulties in cognitive processing, likely as a result of competing demands in the brain. Previous research suggests that pain contributes to cognitive load, or how much information can be processed at any given time, such that it increases activity across different cortical networks in a dysfunctional manner. One subcortical nucleus in particular called the claustrum, may be key to understanding cortical network disruptions related to chronic pain, as this region has been shown to respond to acute pain and shares vast structural and functional connections with the rest of the brain. In a sense, the claustrum may be a “hub” for different functional brain networks whose function is disrupted by chronic pain, such as in patients with migraines. This week in Current Biology, Stewart and colleagues aimed to further characterize the role of the claustrum in response to pain, by investigating how it modulates patterns of brain connectivity during cognitive task performance.
How did they do it?
The authors conducted a series of analyses on functional magnetic resonance imaging (fMRI) data from both patients with migraines and healthy participants. First, the authors looked at the functional activity of the claustrum while healthy participants were exposed to heat stimulation on their forearm, to determine whether it scaled with pain experienced by participants in response to the stimulation compared to other neighboring brain regions. Next, they examined how claustrum responded to auditory cues that would predict the onset of painful heat stimulation in another set of healthy participants. This approach allowed the authors to determine if claustrum is responsive to pain-predictive cues, not just the pain itself. After examining the claustrum in the context of healthy participants, the authors shifted focus to a group of migraine patients, using a cognitive task to probe whether patients would show greater cortical network activity compared to healthy participants. This cognitive task called the multi-source interference task, required participants to identify a unique number in an array. Finally, they used a series of complex statistical approaches, including Partial Least Squares and Dynamic Causal Modeling, to model differences in patterns of functional brain connectivity related to cognitive performances among healthy controls and migraine patients.
What did they find?
The authors found that in healthy adult participants the claustrum, especially in the left hemisphere, is responsive to the experience of heat pain and to cues associated with the onset of heat pain. Subsequently, when the authors compared patterns of activity in brain networks supporting cognitive performance between healthy participants and migraine patients, they found dysfunctional increases in activity among migraine patients. Importantly, these large-scale brain networks, such as the Fronto-Parietal Network, have been shown to have strong functional connections with the claustrum. Among patients with migraines, the authors found that right claustrum activity was significantly greater than that in healthy controls during pain stimulation and cognitive task performance. Finally, they also reported strengthened underlying projections in migraine patients from the right claustrum to a dorsolateral prefrontal cortex region associated with processing pain, even when the migraine patients were pain-free, consistent with a pattern of pathological engagement of the claustrum with chronic pain. These projections were confirmed structurally using diffusion-weighted imaging, a neuroimaging approach that allows researchers to map the movement of water molecules in brain tissue.
What's the impact?
This study found that the claustrum, a subcortical nucleus involved in modulating different cognitive networks of the brain, is activated by acute pain in healthy individuals and is dysfunctional in patients with chronic pain. Altogether, the results of this study overwhelmingly implicate the claustrum in the relationship between cognitive impairment and chronic pain. Understanding chronic pain and finding ways to treat it is important, as an estimated 3.1 billion people globally suffer from chronic headache disorders like migraines, as well as countless more who experience other forms of chronic pain.