Brain Beta-Amyloid Levels Increase after Sleep Deprivation
What's the science?
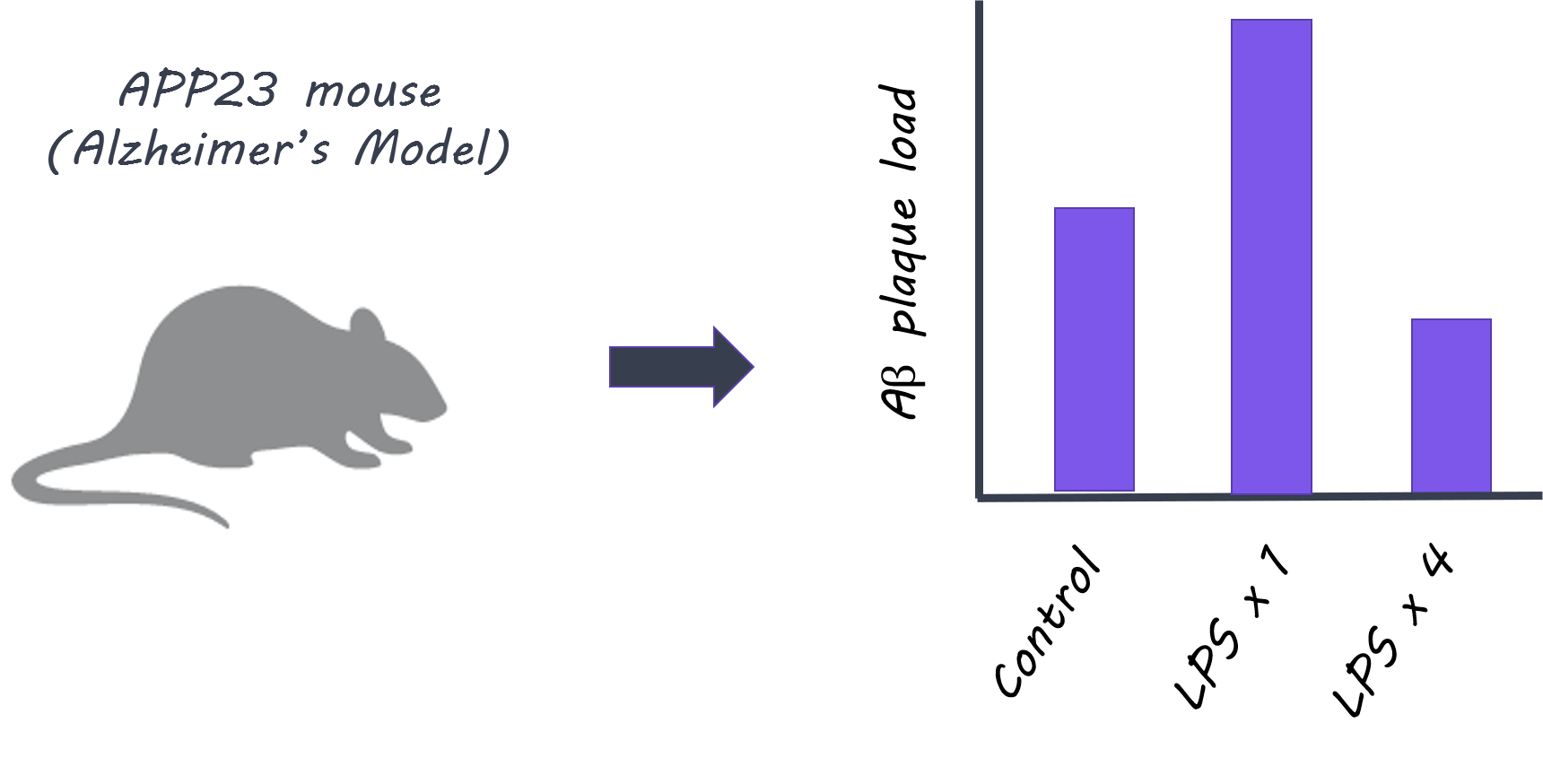
Beta-amyloid is a protein that accumulates in the brain in Alzheimer’s disease and with aging. Sleep is thought to be important for clearance of beta-amyloid as a “waste product” and a lack of sleep over time has been associated with higher beta-amyloid in the brain. There is evidence that beta-amyloid is elevated in brain fluid in mice after acute sleep deprivation, however, it is not clear how acute sleep deprivation affects beta-amyloid levels in the human brain. This week in PNAS, Shokri-Kojori and colleagues use Positron Emission Tomography (PET) to assess whether beta-amyloid is elevated after short-term sleep deprivation in humans.
How did they do it?
PET imaging with a radiotracer called 18F-florbetaben which binds to beta-amyloid in the living human brain, was used to measure beta-amyloid levels in 20 healthy participants. Participants were scanned once after a healthy night of sleep and once after a night of sleep deprivation (no sleep) to compare beta-amyloid levels with and without proper sleep. Participants were given questionnaires related to their mood. Data about sleep history and quality were also collected. The authors hypothesized that beta-amyloid levels would be higher in the hippocampus (one of the first brain regions affected by Alzheimer’s disease) after one night of sleep deprivation and that a poor sleep history would be associated with higher beta-amyloid in brain regions known to be affected by Alzheimer’s disease: the medial prefrontal cortex, the hippocampus and the precuneus.
What did they find?
Beta-amyloid accumulation (measured with 18F-florbetaben) was higher in the right hippocampus after one night of sleep deprivation compared to after a good night’s sleep. The extent to which beta-amyloid increased varied between individuals. Mood was found to be worse after sleep deprivation, and this was correlated with the level of beta-amyloid in the regions showing elevated beta-amyloid such as the hippocampus. Reported hours of sleep per night was negatively correlated with beta-amyloid accumulation (i.e. higher sleep, lower beta-amyloid) in the right hippocampus and thalamus where acute sleep deprivation effects were seen. In a separate whole-brain regression analysis, hours of sleep was also negatively correlated with beta-amyloid levels in the putamen, parahippocampal gyrus and right precuneus (brain regions affected by beta-amyloid in Alzheimer’s disease) confirming that these are key regions affected by hours of sleep.
Brain, Servier Medical Art, image by BrainPost, CC BY-SA 3.0
What's the impact?
This is the first study to show that one night of sleep deprivation is associated with higher beta-amyloid in the human brain. This study also highlights the relationship between hours of sleep (self-reported sleep history) and beta-amyloid accumulation. This study emphasizes that sleep is important for regulating beta-amyloid levels and that sleep deprivation could be one risk factor for brain protein accumulation in Alzheimer’s disease and aging.
E. Shokri-Kojori et al., β-Amyloid accumulation in the human brain after one night of sleep deprivation. PNAS (2018). Access the original scientific publication here.